A Novel Approach to Treating Solid Tumor Metastasis
Patients with liver metastasis face a dire prognosis, with just 10% to 20% surviving 5 years. As a result, liver metastasis has emerged as the leading cause of cancer-related death. Although immune checkpoint inhibitors (ICIs) improve overall survival for many cancer types, they have limited efficacy in solid tumors. Cancers with liver metastasis are often unresponsive to immunotherapy because the liver tumor microenvironment is particularly adept at evading an antitumor immune response.
Survival over 5 years
in patients with cancers that have metastasized to the liver
Many patients will face Liver metastasis…
Most patients with metastatic colorectal cancer (mCRC)—the third most common cancer in men and the second most common cancer in women—will face liver metastasis. Of these, only 4% with DNA mismatch repair defects respond to anti-PD-1 ICIs. The remaining 96% of patients with mCRC are treated with conventional chemotherapy along with targeted agents, such as VEGF or EGFR inhibitors.
mCRC IS THE
most common cancer in men
most common cancer in women
But Have Limited TREATMENT Options
Once these patients have failed 2 lines of chemotherapy, their chance of responding to additional chemotherapy or immunotherapy hovers around 2%, with a median overall survival of 7 months. This leaves a cohort of patients with mCRC in need of a more effective treatment approach.
Chance of response
in patients with cancers that have metastasized to the liver
From Lung to Liver, Options Are Limited
Approximately 30% of patients with lung cancer—the second most common cancer— face liver metastasis with a poor prognosis and limited response to anti-PD-1 ICIs. Those whose cancers progress after treatment with a suitable targeted agent face diminishing returns with additional aggressive chemotherapy and need a better approach.
Of PATIENTS WITH
LUNG CANCER
face liver metastasis
and diminishing returns
Anticancer Immunity
By Inducing solid tumor necrosis, We take a different approach
Because the liver’s strong immune-suppressive environment protects metastatic tumors, current chemotherapies lead the body to develop immune tolerance to the tumor by activating M2 macrophages (immune cells with high immunosuppressive functions). In contrast, when M1 macrophages are activated, they present tumor antigens to the immune system and can induce robust and durable antitumor immunity.
We have pioneered a new strategy that avoids apoptosis and induces tumor necrosis. In doing so, we induce M1 inflammation, attracting extra-hepatic M1 macrophages to the necrotic tumor. This novel approach works with FDA-approved ICIs to induce solid tumor necrosis and boost anticancer immunity.
Our novel hypoxia-activating agent is delivered directly to the tumor through a tumor-feeding artery, creating a hypoxic environment optimal for tumor necrosis. Optimizing the tumor microenvironment for drug activation offers the potential to reach more patients.
This necrosis-triggered inflammation then utilizes macrophages that present tumor-specific antigens to key immune cells. The anticancer immune response works synergistically with an ICI to target other cancer cells throughout the body, including cancer stem cells. Our novel approach can offer immunity against future cancer cell growth and promote lasting remission.
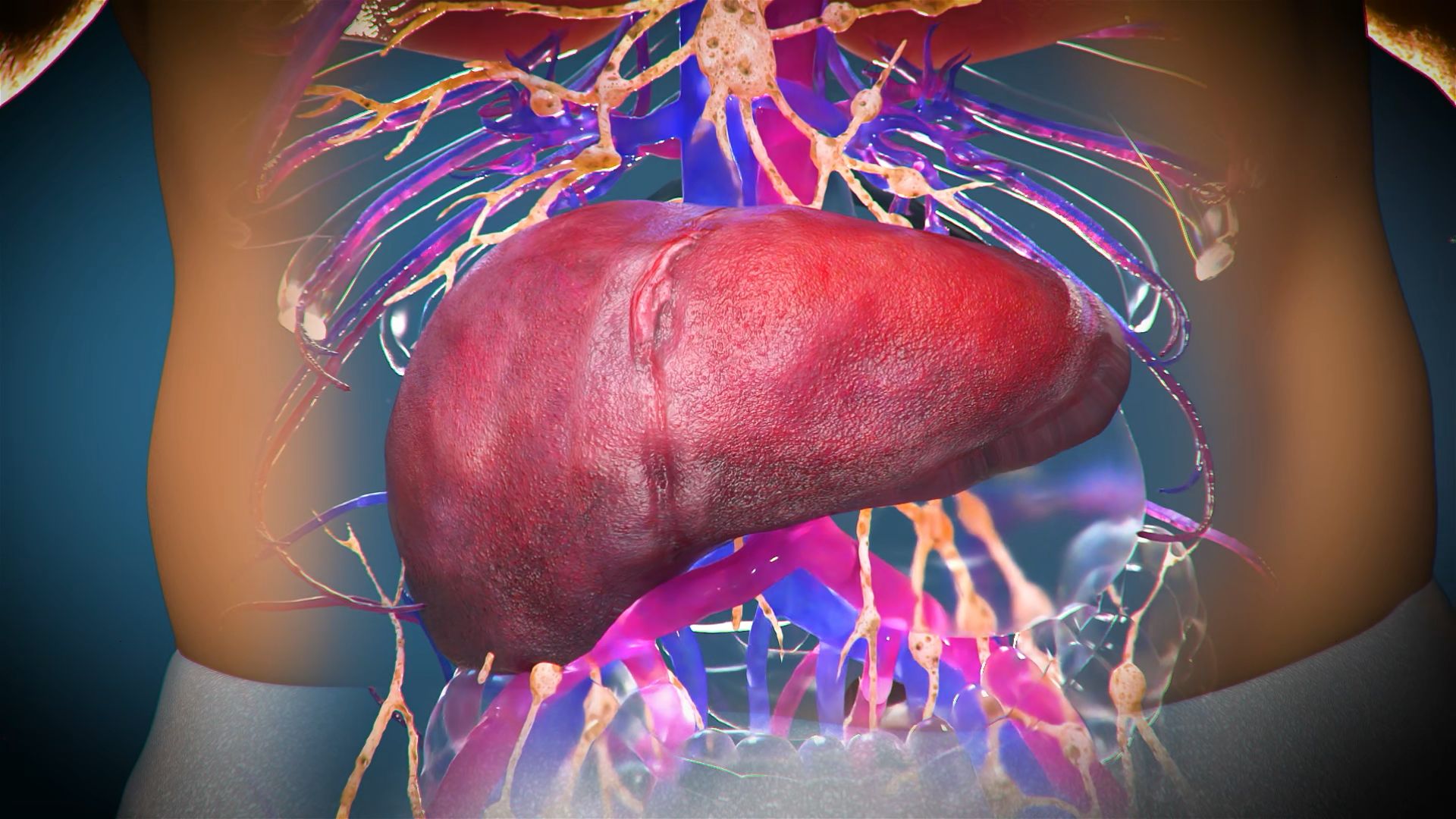
Teclison’s novel, hypoxia-activating agent enables tumor necrosis to reduce liver tumor burden and stimulate the immune system to generate antitumor T-cells that help fight cancer throughout the body.
Key Clinical Evidence
Enhanced Efficacy
Complete tumor necrosis occurred in 60% of patients with intermediate-stage liver cancer treated with our transarterial embolization (TATE) platform therapy, resulting in 52 months of survival compared with 20 to 24 months in those treated with standard of care (SOC).
Proven Safety
Our treatment is only activated under the low-oxygen (hypoxic) condition of a tumor, rendering it harmless to healthy tissues. This approach was well-tolerated in patients with no serious drug-related adverse events reported.
To learn more about our clinical trials, read our publications.


